India is Ageing Faster Than We Think: Why Geriatricians Are the Future Family Physicians
Insights from UNFPA Reports 2017 vs 2023
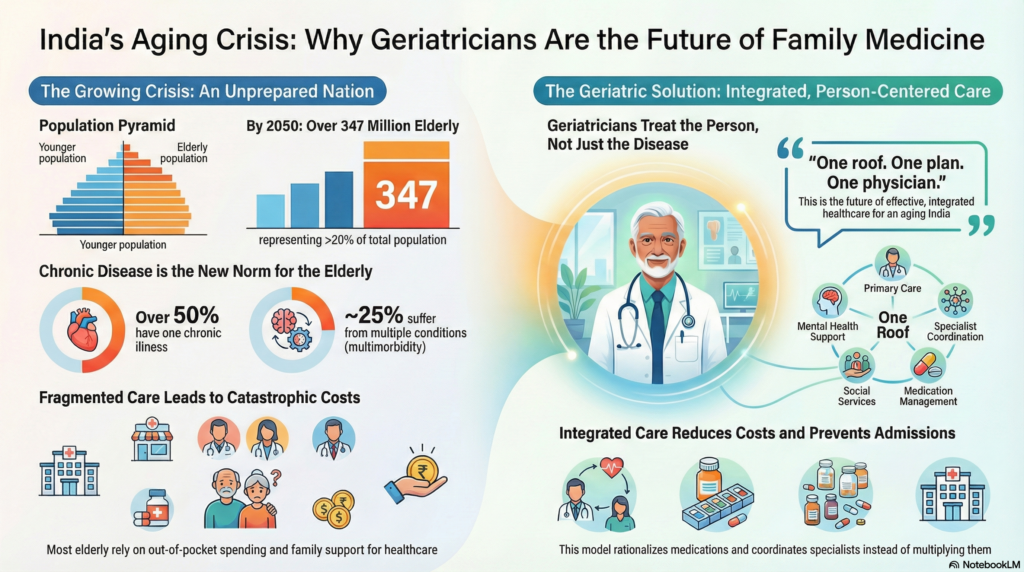
India is experiencing a significant demographic shift. The transition from a “young nation” to an ageing society is clear. This change affects demographics, health, and the economy.
-
Demographic Shift: From Ageing to Rapid Ageing
- Population ≥60 yrs: 104 million (8%) in 2017 to 149 million (10.5%) in 2023.
- Projected ≥60 yrs by 2050: 20% in 2017 to 20.8% (347 million) in 2023.
- Doubling time of elderly: Gradual in 2017 to ~15 years (rapid) in 2023.
- Southern states: Early ageing in 2017 to one in 5 elderly by 2036.
India will soon have more elderly than children. The pace of ageing in India is faster than income growth, unlike in high-income countries.
-
Disease Burden: From Single Illness to Multimorbidity
- 2017: Focused on individual chronic diseases with limited national data on functional decline.
- 2023: Over 50% of older adults have at least one chronic illness, and ~25% have two or more chronic conditions. High prevalence of hypertension, diabetes, arthritis/osteoporosis, cardiovascular disease, depression, and dementia. Functional decline (ADL limitation) in 1 out of 5 elders. Women show higher morbidity, disability, and widowhood.
This is not organ-based disease; this is syndrome-based ageing.
-
Health Burden: The Missing Middle of Care
India’s system is currently designed for acute care, single-organ specialties, and episodic treatment. But ageing brings polypharmacy, frailty, falls, cognitive impairment, nutrition decline, and social vulnerability. The 2023 report highlights that integrated, continuous, person-centred care is largely missing, especially at the primary and secondary levels.
-
Health Economics: Ageing = Catastrophic Expenditure Risk
Key findings (2023):
- Majority of elderly depend on out-of-pocket expenditure and family support.
- Low pension coverage, especially among women.
- High costs due to multiple consultations, repeated investigations, fragmented care, and poor insurance penetration for chronic Geriatric needs.
Uncoordinated care is expensive care.
-
Why Geriatricians Are the New Family Physicians
India once relied on the family physician model. Ageing demands its modern equivalent. A Geriatrician treats the person, not organs, manages multiple diseases in one visit, rationalises medications, and integrates medical care, functional care, mental health, and social context. They prevent unnecessary admissions, reduce healthcare costs, and coordinate specialists instead of multiplying them.
One roof. One plan. One physician. This is exactly what the UN Decade of Healthy Ageing calls integrated care.
-
Geriatrics Is Not Optional : It Is Inevitable
The 2023 report clearly signals that India cannot afford fragmented elder care. Geriatrics must move from tertiary hospitals to primary and community care. Geriatricians will anchor health systems, long-term care, home-based care, and policy design. Geriatrics is not a niche. It is the backbone of future Indian healthcare.
Conclusion
India is ageing faster than its systems are adapting. The choice is simple: reactive, expensive, fragmented care or preventive, integrated, geriatric-led care. The future belongs to Geriatricians as Family Physicians for an ageing India.
Dr Manicka Saravanan S
Consultant Geriatrician
Dr M S clinic, For Appts: 9600925266